Mastering Payment Collection and A/R in Medical Billing
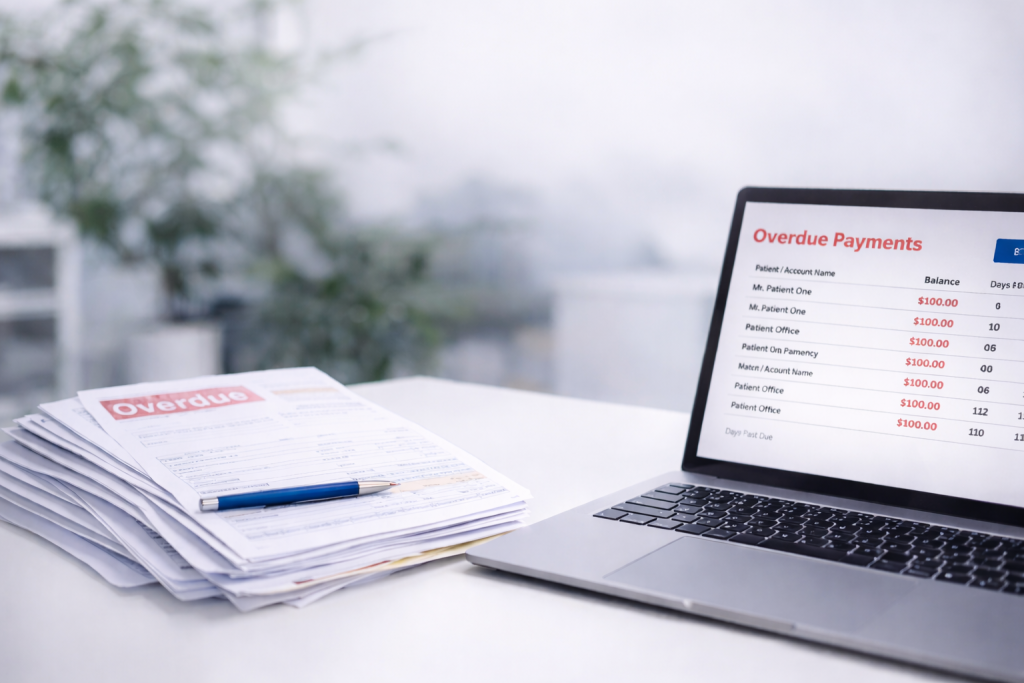
The Hidden Cost of Inefficient Payment Collection
Every day a claim sits unpaid, your cash flow suffers. For healthcare providers and billing firms, delayed payments and ballooning A/R days aren’t just operational issues — they’re symptoms of systemic inefficiency. Industry data shows that up to 25% of claims require rework, and 65% of denied claims are never resubmitted. Those numbers translate directly to lost revenue.
YZK’s payment collection and A/R solutions were built to solve exactly this — automating workflows, tracking denials, and recovering revenue that most billing teams write off as uncollectible.
Understanding the A/R Lifecycle in Medical Billing
Accounts Receivable management in healthcare is uniquely complex due to multi-payer systems, frequent denials, and evolving payer rules. YZK blends expert RCM strategy with proven process management, ensuring every claim moves seamlessly from submission to settlement. Our experts monitor aging buckets, denial trends, and payer behavior — giving you visibility and control over every dollar owed.
Most medical practices struggle to maintain efficient A/R cycles because of fragmented workflows, inadequate follow-up systems, and manual reconciliation. YZK addresses these challenges with a proactive, process-driven approach that keeps claims moving through the pipeline.
The YZK Method: Turning A/R into Predictable Revenue
- Automated Follow-ups: Smart triggers ensure no claim goes cold.
- Real-time Payment Posting: Insurance and patient payments are reconciled efficiently.
- A/R Intelligence Dashboard: Track performance by payer, claim type, or date of service.
- Compliance-Ready Workflows: Built-in HIPAA and payer rule validation reduce rejections.
- Specialized Expertise: Our billing team understands payer behavior across every specialty.
It’s human intelligence, experience, and precision — designed by professionals who understand medical billing down to the CPT code level.
YZK continuously refines its workflows based on historical claim data and client feedback, improving collection speed, accuracy, and overall efficiency without relying on AI or automation hype. Our methods are rooted in accountability, transparency, and proven operational excellence.
Common Challenges in Payment Collection and How YZK Solves Them
- Denied Claims: YZK’s denial management system categorizes denials, identifies trends, and ensures timely re-submission — reducing write-offs dramatically.
- Patient Payment Delays: Our integrated patient billing portal makes it easy for patients to view and pay balances online, improving collection rates.
- Lack of Visibility: With detailed analytics, billing managers can view KPIs in real time — such as aging by payer, claim turnaround, and payment variance.
- Staff Overload: YZK simplifies repetitive tasks, freeing your staff to focus on high-value recovery efforts and patient satisfaction.
Proven Results for Healthcare Providers
- 40–60% faster claim resolution
- 25% improvement in first-pass acceptance rate
- 35% reduction in A/R days
- Significant increases in cash flow and staff productivity
Our mission is simple: make your revenue predictable, transparent, and scalable.
With a data-driven foundation and deep domain expertise, YZK ensures that every aspect of your revenue cycle is optimized for speed, accuracy, and compliance. Whether you’re managing a single specialty clinic or a multi-location practice, our platform adapts to your unique operational needs.
Why YZK Leads in Healthcare A/R Management
YZK isn’t just a billing service — we’re a strategic partner. Our team of certified medical billing specialists, financial analysts, and RCM experts work alongside clients to achieve sustainable revenue growth. By combining advanced systems with experienced professionals, we help practices build long-term financial resilience.
YZK’s proprietary workflow engine identifies payer trends, detects payment anomalies, and helps prioritize high-value claims for faster reimbursement. This ensures minimal delays and keeps your revenue flowing consistently.
We also offer continuous support, including regular performance reviews, benchmarking reports, and compliance audits, ensuring that your organization stays ahead of evolving regulations and payer policies.
Looking Ahead: The Future of A/R in Medical Billing
The medical billing industry is evolving rapidly, driven by stricter compliance rules, payer digitization, and growing patient financial responsibility. YZK stays ahead by continuously refining our processes, investing in staff training, and adapting our tools to new payer environments.
From improved electronic claim submissions to transparent patient billing and follow-up workflows, YZK ensures that our clients remain equipped for a future where efficiency, accuracy, and transparency define financial success.
Take Control of Your Revenue Cycle
Your team shouldn’t be chasing payments — your system should. Partner with YZK and transform your A/R management from a reactive process into a strategic advantage.
